In the evolving landscape of Veterinary Orthotics and Prosthetics (VOP), the quest for the most effective and efficient method of capturing the unique contours of an animal’s limb for orthotic or dog prosthetic fabrication has been ongoing. Explore the limitations of conventional casting methods and discover WimbaSCAN for precise and efficient pet orthotics solutions.
For many years VOP has relied on conventional impression acquisition methods like Plaster of Paris (POP) and fiberglass casting, as the foundational techniques for capturing the shape of an animal’s limb. The common plaster-of-Paris cast was first used in the middle of XIX century (precisely 1852 by Methijsen) [SZO2017]. Fiberglass casting tape was introduced in the 1970s [HAR2006]. Synthetic casts (cotton or fiberglass bandage with polyurethane resin) seem to have superior properties with regard to lamination and curing time [ROW1985] and are generally easier to apply and do not mess. However, one should consider the higher cost of fiberglass and the fact that precise molding is more difficult with synthetic casts [DAI2014]. Although there is a lack of robust evidence, the potential toxicity of synthetic casting materials is of concern. Nevertheless, these two materials are still the most widely used today in VOP.
These methods have been the mainstream due to their proven utility over time and with absence of better, digital alternatives. However, the landscape began to evolve with the introduction of more modern technologies such as structured light scanners and Lidar technology. Initially adopted in human Orthotics & Prosthetics (O&P), these newer techniques promised enhanced precision and efficiency but also introduced a new set of challenges when applied to veterinary practice.
There has been a growing recognition within the veterinary community of the inherent limitations associated with both traditional casting methods and those technologies directly adapted from human O&P. The traditional techniques, while familiar, are often time-consuming and may not always capture the intricate details necessary for optimal orthotic or prosthetic fitting. On the other hand, traditional human O&P scanning technologies like 3D scanning, though effective in delivering high precision, often fall short in veterinary settings due to their significant costs, design considerations tailored for larger human body parts, and a heavy reliance on the subject’s ability to remain still. Such conditions are rarely met in veterinary practice, where the subjects are often smaller, less cooperative animals, making these technologies less practical for routine use. This acknowledgment of the gaps in existing methods led to the conceptualization of a new method.
WimbaSCAN is distinct from the impression acquisition methods traditionally employed in VOP and those adapted from human O&P. Its conception was driven by the need for a bespoke solution that addresses the unique requirements of animal care, rather than replicating technologies designed elsewhere. It is not merely another addition to the existing array of methods but rather introduces new possibilities that transcend the current concepts. The approach acknowledges and addresses several critical areas.

1. User – Vet Professionals
Consider the fact that veterinarians, while experts in animal health, may not possess specialized skills in traditional O&P techniques such as molding or using fiberglass, nor are they typically trained in utilizing complex 3D scanning equipment. Maybe we could simply address this gap by harnessing a skill most veterinarians are already familiar with: capturing video footage using a smartphone. This method ensures that the technology is not only accessible (this technology democratizes the process!) but also does not require veterinary professionals to undergo extensive training in unfamiliar techniques nor buy expensive equipment. Keep in mind that the goal is to seamlessly integrate into an existing practice. The ease of capturing a video, as opposed to conducting a full 3D scan or creating a physical mold, represents a significant reduction in the procedural complexity and technical skill required.
2. Resources
In veterinary clinics, where every minute counts, saving time is crucial. Traditional casting methods, while tried-and-true, can be pretty hands-on and messy. On the flip side, those high-tech 3D scanners, though precise, can hit the wallet hard and take up too much time to set up and use. The ideal solution would make gathering the needed data quick and smooth, allowing veterinarians to dedicate more time to patient care rather than dealing with cumbersome casts or complex scanning procedures. Isn’t video recording with our smartphone precisely the solution we’re looking for?
3. Medical Accuracy
Traditional methods of limb impression in VOP have long focused on replicating the current state of an animal’s limb, which more often than not reflects a compromised condition due to injury or disease. Moreover, techniques like fiberglass casting typically require the animal to be under sedation to achieve the necessary stillness for accurate molding. This approach, while practical in some respects, overlooks a critical aspect of animal behavior: their inherent dynamism. Animals are naturally active, engaging in a variety of movements such as running, playing, and grazing. This constant motion is a fundamental part of their existence and should be a consideration in the design of orthotic and prosthetic devices.
Recognizing this, the WimbaSCAN technology offers a significant advancement by allowing for the capture of multiple video recordings, showcasing the limb in various states of load and unload, and even comparing it to the corresponding healthy limb. This multifaceted view enables a comprehensive understanding of the limb’s functional dynamics and the ultimate goal of rehabilitation.
Further enhancing this approach is WimbaSCAN’s allows for the morphing of the 3D model based on key anatomical landmarks and a “virtual kinematic chain.” This innovative feature allows for the transformation of the model to not just mirror the current state of the limb but to envision and design for the limb’s optimal, healthy state post-recovery. The focus shifts from merely accommodating the limb’s present condition to actively supporting its healing process. This forward-thinking methodology underscores a commitment to not just the immediate needs of the animal, but to its long-term health and mobility, aligning with the ultimate goal of veterinary care: to restore and enhance the quality of life for animal patients.
4. Patient Comfort
Ensuring the comfort of our animal patients during the impression-taking process is paramount, particularly since traditional casting methods can be invasive and potentially add stress, especially for those already in discomfort. A major concern with conventional approaches is their reliance on sedation, which can be intolerable for some animals and pose unnecessary health risks. Additionally, an animal’s fur can significantly impact the accuracy of 3D impressions, often requiring the removal of fur, which can be another source of stress for the patient. Let’s keep the well-being of the animal at the forefront. It should also be acknowledged that sedation significantly reduces muscle tone, thereby altering the physiological contour of the leg. Conversely, animals not under sedation may exhibit increased muscle tone, which influences both the muscle structure and the positioning of the leg.
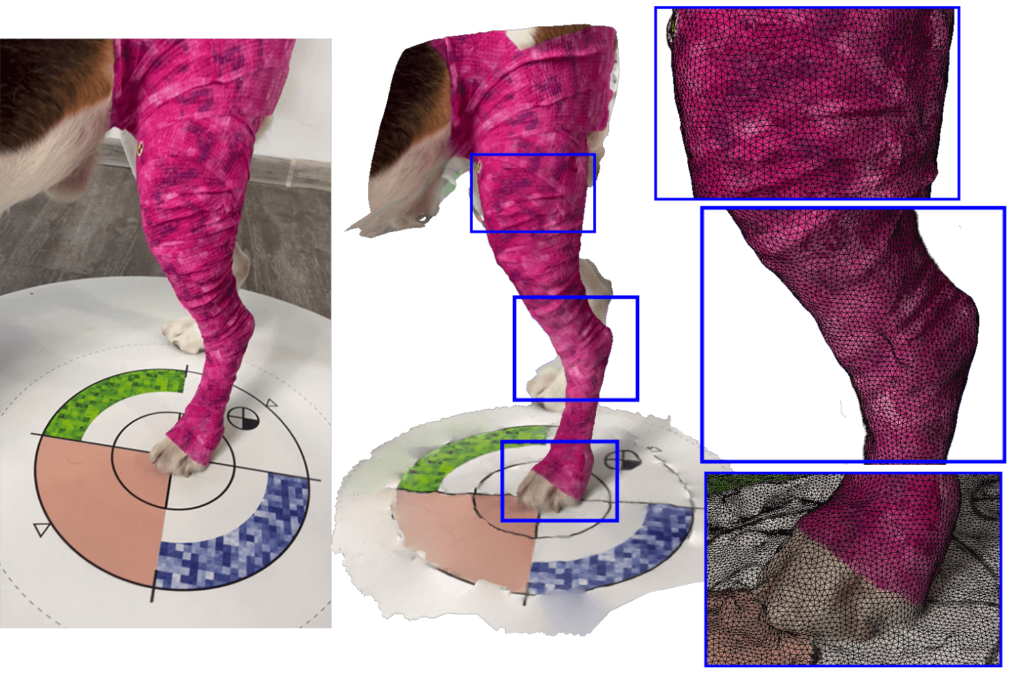
To tackle these challenges in a non-invasive way, WIMBA with the innovative shape WimbaSCAN shape acquisition method has introduced a specially designed sleeve-like device that streamlines the process. This solution is tailored to snugly fit over the animal’s limb, effectively minimising fur interference in the shape acquisition process. The beauty of this solution lies in its simplicity and it negates the impact of fur on scanning quality, ensuring accurate captures without the need for sedation or the discomfort associated with fur removal.

5. Precision
When discussing the accuracy of replicating a dog’s limb shape by PoP or casting, the conversation often lacks quantifiable data, resorting instead to vague descriptions such as ‘good’, ‘average’, or ‘poor’. To truly understand the factors contributing to precision, a deeper analysis is necessary.
Firstly, in traditional fiberglass casting, the fidelity of the resultant shape can vary significantly based on several factors. The ‘sculpting’ skill of the veterinarian plays a crucial role, likening the process more to an art form than a precise science. The size of the dog also impacts the difficulty level of the casting process—the smaller the dog, the greater the challenge. Additionally, the cooperation of the animal during the casting process, ensuring it remains still, is a critical factor, among others. Anyone who has attempted to cast a dog’s leg even once understands the inherent challenges and complexities of the task.
It’s widely acknowledged that a fiberglass cast is inherently less accurate than a POP cast, a point on which there is global consensus. The journey from the veterinary clinic further complicates matters. Even if a cast is exceptionally well-made, it must undergo shipping, transportation, and unpacking, followed by the creation of a gypsum positive mold based on the cast to obtain a model of the limb. This model serves as the foundation around which the orthotic device is constructed. In some facilities, this stage may also involve professional 3D scanning to further refine the design process. Each step in this process introduces potential errors, whether intended or not. Consequently, a well-crafted cast may lose some of its precision by the end of this journey, whereas a poorly made cast might bear little resemblance to the original shape of the dog’s paw. In such cases, the only solution for improvement is often to redo the cast entirely. This inherent inaccuracy in traditional orthotic fittings is why the term “Adjustments” frequently arises. More often than not, these devices do not fit perfectly and must be accepted with a degree of tolerance for imperfection, necessitating further adjustments to achieve an adequate fit.
6. WimbaSCAN Technology Behind the Curtain
Intense research in the computer vision community has led to a wealth of image-based reconstruction and modelling systems that take images as input and construct a detailed 3D model of the scene [SZE2010]. From the perspective of accurately capturing the shape of an animal’s limb—and crucially for the discussions in this article—the most essential technologies are Structure-from-Motion (SfM) and Multi-View Stereo (MVS). These tools, falling under the broad umbrella of techniques known as photogrammetry, are capable of reconstructing a geometrically precise model that includes texture and colour details. Furthermore, thanks to recent significant improvements in hardware and algorithms, photogrammetry has re-emerged as a competitive technology [SCH2016]. Video-based AI/ML systems (e.g. metaverse avatar [MA2021]) and 3D modelling can now deliver, in unbelievable short time, results of comparable or better geometric characteristics to those of laser scanning. Therefore, the market, which was previously primarily dominated by range sensors, nowadays offers more image-based measurement tools for 3D recording and modelling.
The advent of AI and ML techniques has dramatically transformed this landscape, unlocking a plethora of new possibilities. How does the process work? We assume that the input is a video showing an animal body, changing pose over time due to camera motion. The reconstruction is performed using an SfM-based approach, aiming to produce 3D shapes that are true to the actual shapes of the animal limbs. SfM methods necessitate sufficiently high-resolution images, a criterion met by HD quality videos. However, photogrammetry faces its own set of challenges, including the animal’s movement, fur that obscures views during motion, and a scarcity of key features. From an algorithmic standpoint, homogeneous animal regions can lead to ambiguous matches, significantly degrading the quality of the reconstructed 3D shapes. To mitigate these problems, we propose leveraging knowledge about the shape being scanned by introducing special patterns and utilizing statistical shape analysis. This not only facilitates the feature tracker’s task but also dramatically improves accuracy.
Discover WimbaSCAN leveraging Augmented Reality (AR) technology here.



Let’s delve into the realm of precision & accuracy by referencing research conducted over many years in various scientific domains, particularly in human medicine. The integration of the SfM technique marks a significant leap forward in the field.
In 2018, Maureen Ross conducted a study examining various scanning techniques, including the feasibility of using a smartphone to create accurate scans of human faces with 30-60 photographs [ROS2018]. This investigation demonstrated that smartphone photogrammetry could achieve accuracy, completeness, and repeatability comparable to those of more expensive 3D scanning technologies. Moreover, the cost associated with this method was significantly lower, less than 1% of the cost of higher-end 3D scanners at that time. The reported reliability of this method, as indicated by a root mean square (RMS) error of 1.0 ± 0.1 mm.
In the 2021 study by Night investigated the use of smartphone cameras for clinical 3D scanning of the external ear. Even novice operators, after a brief instructional session, were able to produce accurate and reliable 3D scans using a smartphone-based SfM approach. The scans were found to be accurate within 1.5 ± 0.4 mm when compared to a gold standard reference scanner [NIG2021].
The accuracy of SfM is not constrained by the limitations often associated with laser scanning, but rather by the resolution of the video used. This attribute enables the achievement of high precision in model reconstruction. In 2021 SfM was applied to digitalize human pelvis, yielding surface representations with average deviations 0.2 mm when compared to models obtained via traditional methods like CT and structured light scanning [WAL2021]. Results were achieved with rigorous laboratory setup but this showcases the potential of SfM as a tool for detailed anatomical modelling.
More and more studies have shown that recently SfM is the most used and most suitable 3D scanner for the acquisition of the human body in 3D (see [PAX2022], [CUL2023]). The WimbaSCAN approach, inspired by these advancements, aims to harness the precision and accessibility of photogrammetry and SfM for the VOP sector. As technology advances, it becomes feasible to reduce scanning and processing times, enhance accuracy, and widely integrate this technology into clinical settings.

7. The Power of Kinematics…
In the realm of veterinary orthopedics, particularly concerning the management and correction of limb functional deformities in dogs, the concept of kinematic chains plays a pivotal role in understanding and addressing the complex dynamics of leg movement and positioning. A kinematic chain refers to a sequence of rigid body segments connected by joints, allowing for motion. This framework is crucial when examining how alterations in one segment of a dog’s leg can influence the entire limb’s alignment and function.
Building on this foundational understanding, we utilize algorithms based on kinematic chain principles to refine the leg’s positioning in anticipation of applying an orthotic solution.
Imagine a scenario in which the scanning process introduces some modifications, as depicted in the graphic (nr. graphic), in which the scanned leg exhibits an increased flexion at the stifle due to pre-existing conditions, rather than normal standing position.
Upon confirming the correction’s viability, the algorithm adjusts the 3D scanned pathological position of the dog’s leg to a preplanned, anatomically sound configuration.
This recalibration process is pivotal, as it ensures that the design of the orthotic device is based on the planned anatomical alignment rather than the existing pathological condition. Consequently, this sophisticated approach not only enhances the accuracy of orthotic fitting but also optimizes the therapeutic benefits, promoting a more natural and efficient gait in the affected canine.
8. WimbaSCAN Conclusions
The traditional method of building custom-made orthoses with plaster casts has remained largely unchanged despite the introduction of new technologies which aid post-processing. With today’s advancements such as WimbaSCAN, there is an opportunity to transition from the traditional method to one that better meets the needs of patients and professionals. Maybe the future is now and with right, easy, affordable scanning technology digitalization of orthotics and integration into clinics becomes finally feasible and possible.
From a technical point of view, the resolution of the images produced with Machine Learning techniques combined with photogrammetry is much higher than that produced by high-precision laser scanners. Related technologies are materializing and poised to profoundly change how we utilize 3D data in VOP.
WimbaSCAN is a standalone, easy-to-use solution for precise data acquisition, enabling automated limb reconstruction and optimal product fit.
- WimbaSCAN enables data acquisition for taking digital measurements of limbs and creating digital models.
- Digital limb reconstruction for dogs has been automated through the use of advanced image processing algorithms.
- Shape analysis algorithms ensure proper product fit and comfort.
Discover the Power of WimbaSCAN Today!
Ready to revolutionize your practice? Experience the precision and efficiency of WimbaSCAN. Don’t wait—order your WIMBA orthotics products now and see the difference they can make!
Authors
Dr. Kuba Letek, DVM, Medical Chief Officer
Rafał Michalczyk, PhD, Head of Technology Initiative
REFERENCES
SZO2017; Szostakowski, B., Smitham, P., & Khan, W. S. (2017). Plaster of Paris–short history of casting and injured limb immobilzation. The Open Orthopaedics Journal, 11, 291.
HAR2006; Harness, N. G., & Meals, R. A. (2006). The history of fracture fixation of the hand and wrist. Clinical Orthopaedics and Related Research (1976-2007), 445, 19-29.
ROW1985; Rowley, D. I., Pratt, D., Powell, E. S., Norris, S. H., & Duckworth, T. (1985). The comparative properties of plaster of Paris and plaster of Paris substitutes. Archives of orthopaedic and traumatic surgery, 103, 402-407.
DAI2014; Daines, S. B., Aronsson, D. D., Beynnon, B. D., Sturnick, D. R., Lisle, J. W., & Naud, S. (2014). What is the best material for molding casts in children?. Journal of Pediatric Orthopaedics, 34(7), 743-748.
SZE2010; Szeliski, R. (2022). Computer vision: algorithms and applications. Springer Nature.
SCH2016; Schonberger, J. L., & Frahm, J. M. (2016). Structure-from-motion revisited. In Proceedings of the IEEE conference on computer vision and pattern recognition (pp. 4104-4113).
MA2021; Ma, S., Simon, T., Saragih, J., Wang, D., Li, Y., De La Torre, F., & Sheikh, Y. (2021). Pixel codec avatars. In Proceedings of the IEEE/CVF Conference on Computer Vision and Pattern Recognition (pp. 64-73).
ROS2018; Ross, M. T., Cruz, R., Brooks-Richards, T. L., Hafner, L. M., Powell, S. K., & Woodruff, M. A. (2018). Comparison of three-dimensional surface scanning techniques for capturing the external ear. Virtual and Physical Prototyping, 13(4), 255-265.
NIG2021; Nightingale, R. C., Ross, M. T., Cruz, R. L., Allenby, M. C., Powell, S. K., & Woodruff, M. A. (2021). Frugal 3D scanning using smartphones provides an accessible framework for capturing the external ear. Journal of Plastic, Reconstructive & Aesthetic Surgery, 74(11), 3066-3072.
WAL2021; Waltenberger, L., Rebay-Salisbury, K., & Mitteroecker, P. (2021). Three-dimensional surface scanning methods in osteology: A topographical and geometric morphometric comparison. American Journal of Physical Anthropology, 174(4), 846-858.
PAX2022; Paxton, N. C., Nightingale, R. C., & Woodruff, M. A. (2022). Capturing patient anatomy for designing and manufacturing personalized prostheses. Current Opinion in Biotechnology, 73, 282-289.
CUL2023; Cullen, S., Mackay, R., Mohagheghi, A., & Du, X. (2023). Low-Cost Smartphone Photogrammetry Accurately Digitises Positive Socket and Limb Casts. Prosthesis, 5(4), 1382-1392.

